1. Introduction
Borderline Personality Disorder (BPD) is a severe and complex psychiatric condition characterised by pervasive instability in emotional regulation, interpersonal relationships, self-image, and impulse control. Individuals with BPD frequently experience intense affective lability, chronic feelings of emptiness, identity disturbance, and recurrent suicidal behaviour or self-injury [
1]. Since the seminal study of Linehan [
2], substantial progress has been made in the therapeutic management of BPD. A large body of evidence has supported the efficacy of structured psychotherapies [
3], and new modalities—both psychological and biological—are continuously emerging. Our understanding of the underlying mechanisms of BPD, its clinical heterogeneity, and the impact on everyday functioning has significantly deepened [
4,
5]. This growing body of knowledge is now shedding lig on specific therapeutic targets [
4,
6,
7]—mortality, symptoms, psychosocial functioning, and social inclusion—which will be explored in the following section, alongside emerging personalised interventions.
Among all treatment priorities, life expectancy stands out as the most fundamental. While death is an inherent part of life, the stark inequalities in life expectancy between individuals with BPD and the general population are both striking and unacceptable [
8,
9,
10]. Reducing this gap is imperative because, without life, no other therapeutic goal retains its meaning. Historically, efforts to extend life expectancy have focused primarily on lowering suicide, which remains the most prominent cause of excess mortality in individuals with BPD compared to the general population [
9,
11]. Consequently, suicide prevention has become a central focus of numerous therapeutic interventions. While several treatments have demonstrated effects on suicidal ideation, self-injurious behaviour, and suicide attempts [
3,
12], it is important to recognise that no intervention to date has shown a definitive impact on reducing suicide mortality itself. Moreover, a critical but often overlooked reality is that most individuals with BPD ultimately die from physical health conditions—many of which are both preventable and more prevalent in this population than in the general population (e.g., cardiovascular disease, substance-related disorders, metabolic syndrome) [
8,
9].
Beyond its potential to mitigate mortality risks associated with both BPD and comorbid conditions, symptom reduction also addresses the core reasons individuals seek psychiatric care, making it a critical therapeutic priority. Treating BPD involves alleviating the emotional distress and functional impairments associated with core BPD symptoms, along with those stemming from common comorbidities. Over the past decades, most clinical studies have focused on reducing BPD symptomatology as the primary treatment target [
3,
13]. However, there is a growing recognition that comorbid conditions—such as depression, anxiety, PTSD, substance use disorders, ADHD and eating disorders—are not only highly prevalent in individuals with BPD [
14], but also significantly influence clinical outcomes, including relapse [
15], quality of life [
16], and suicide risk [
17,
18]. Acknowledging the central role of comorbidities underscores the importance of considering their reduction and management as essential therapeutic outcomes.
The third level of treatment targets broader, person-centred outcomes such as quality of life, sense of purpose, functional recovery, and social integration. For many individuals with BPD, the pursuit of a fulfilling life—encompassing gratifying relationships, stable employment, meaningful activities and projects, and a coherent life narrative—remains a significant challenge [
19] and a goal [
20]. While symptomatic remission is often achievable, complete recovery, defined by both clinical and functional remission, is far less common [
21]. Despite their importance, these outcomes have traditionally been treated as secondary endpoints in clinical research, often overshadowed by symptom reduction and safety measures. This raises important questions about treatment development and evaluation priorities: Are we aiming for mere symptom control or for the possibility of functioning optimally in everyday activities and thriving in a meaningful life? Addressing this gap calls for a shift toward long-term, holistic goals that reflect patients lived experiences and aspirations.
A fourth level of treatment targets operates at the interpersonal and societal level, reflecting the bidirectional relationship between individuals with BPD and their social environment. It is well established that early relational trauma—particularly during childhood and adolescence—plays a central role in the development of BPD [
22]. Later in life, social stigma, especially within healthcare systems, can further exacerbate suffering and reinforce exclusion [
23]. Conversely, BPD significantly affects others. As a disorder fundamentally rooted in interpersonal dysfunction, BPD can place considerable strain on families [
24], partners, children [
25], friends, and professional networks. At a broader level, the disorder poses challenges to healthcare systems and society, contributing to high rates of service use, emotional burden on caregivers, and workplace difficulties [
26]. Acknowledging and addressing this social dimension is essential. Therapeutic innovations must not only aim to support the individual but also repair and strengthen social bonds, reduce stigma, and consider systemic impacts, ultimately fostering healthier relational ecosystems around the person with BPD.
While research continues to provide growing evidence on how best to treat individuals with BPD, efforts often remain fragmented. Each study pursues its own path, focusing on specific aspects of the disorder without contributing to a unified understanding. Despite the clinical and societal burden of BPD, research funding remains limited [
27], and there is currently no coordinated strategy or collective roadmap to address the four central domains of treatment outcomes: premature mortality, symptom reduction, psychosocial functioning, and societal impact. This fragmentation also impacts clinical care [
28]. People with BPD and their families consistently express a desire for high-quality, professional healthcare that is rooted in respect, compassion, and meaningful therapeutic relationships [
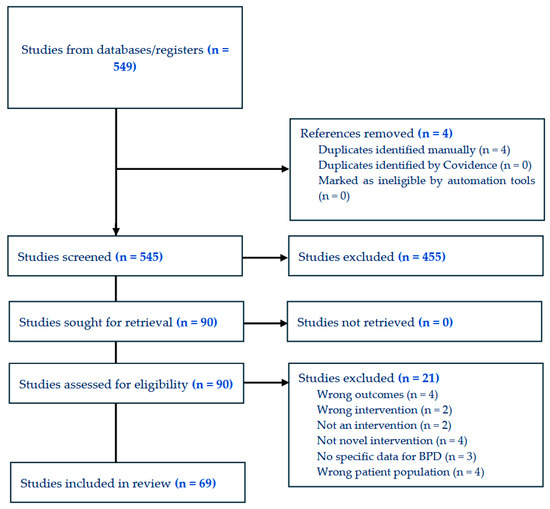
29]. This rapid review examines whether current therapeutic innovations truly reflect and respond to the full complexity of BPD.
The objectives of this rapid review were threefold. First, to systematically identify and classify recent therapeutic innovations for BPD, including novel psychotherapies, pharmacological treatments, digital tools, and neuromodulation techniques, published between 2019 and 2025. Second, to evaluate how these interventions address key clinical and functional outcome domains, such as mortality (e.g., suicide prevention and reduction in physical health-related mortality), symptomatology (targeting core BPD symptoms and common comorbidities), psychosocial functioning (including recovery, quality of life, and global remission), and societal impact (such as stigma reduction, interpersonal relationships, and occupational functioning). Third, this review aimed to identify persisting research gaps and misalignments between current innovation trends and pressing therapeutic needs, to inform future research priorities and promote a more socially responsive and outcome-relevant research agenda.